- Shortness of breath
- Fatigue
- Stomach swelling (ascites)
- Weight gain
- Jugular vein distension
Understanding tricuspid regurgitation
If you or a loved one has symptomatic severe tricuspid regurgitation (TR), please know that you’re not alone and you do have options when it comes to treatment.


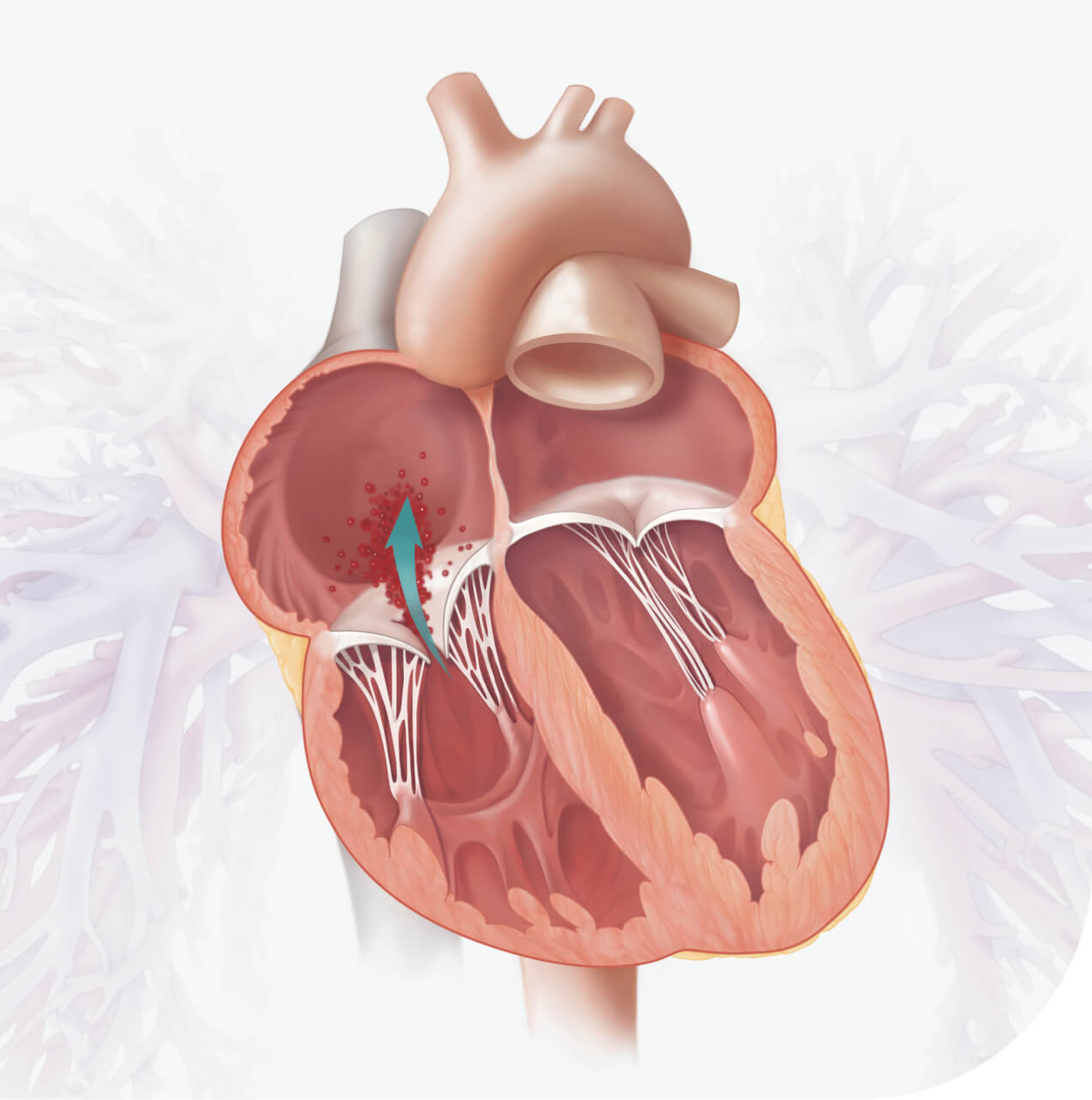
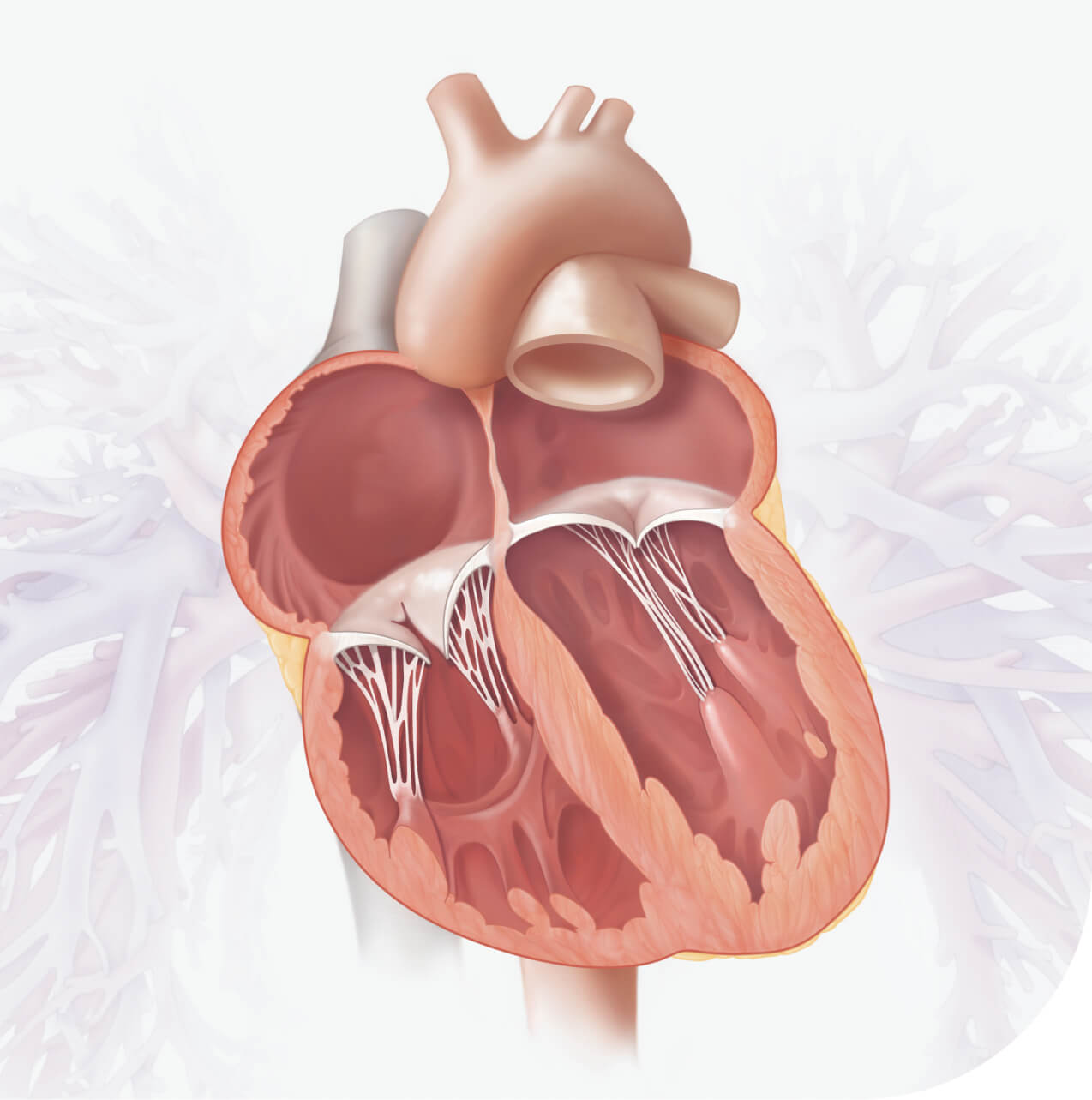
What is Tricuspid Regurgitation (TR)?
Your heart has four chambers and four valves that open and close to keep blood flowing in the right direction.1 The tricuspid valve separates the upper and lower chambers on the right side of your heart. When your tricuspid valve is working properly, it helps you stay healthy and active.2
Over 1.5 million people in the United States
are estimated to have moderate or greater TR3, 4, 5
Symptoms and signs of severe tricuspid regurgitation may include:
- Stomach pain
- Enlarged liver or spleen
- Swollen ankles and feet (lower limb edema)

Severe TR symptoms often lead to a substantial decrease in your quality of life. Activities like taking walks or just moving from room to room can become extremely challenging and limit your independence. Signs and symptoms of severe TR may be mistaken as normal consequences of aging, which can delay treatment.7, 8, 9
What causes tricuspid regurgitation?
The most common cause of tricuspid regurgitation is the enlargement of the right ventricle. The right ventricle normally pumps blood to the lungs where it picks up oxygen. Conditions that put extra strain on the right ventricle can cause it to enlarge.6 This results in a misshapen tricuspid valve that does not close properly and causes blood to flow back into the right atrium instead of being pumped forward into the lungs.
Most common causes:8
- Heart failure
- Pulmonary hypertension
- Cardiomyopathy
TR can also develop due to:7
- Infection, such as infective endocarditis or rheumatic fever
- Congenital heart disease, such as Ebstein anomaly
- Carcinoid syndrome
- Endomyocardial biopsy
- Chest trauma
- Radiation therapy
- Injury caused during the placement or removal of implantable device

What happens if your TR is left untreated?
If you have severe tricuspid regurgitation that isn't getting better with medication, the outlook may not be good without additional care.7 Waiting to get help can make your symptoms worse, limit what you can do every day, and increase the risk of heart failure or even death. If you or someone you care about has ongoing symptoms, talk to your cardiologist about tricuspid regurgitation and check out the treatment options available now.

What are your treatment options?
In the past, treatment options for symptomatic severe tricuspid regurgitation were limited to oral medication and heart surgery. However, a minimally invasive treatment is available. This option for treating tricuspid regurgitation can improve quality of life and offer faster recovery than traditional surgery with lasting relief.10
We’re here for you
Whether you’re looking to learn more about your condition, explore treatment options, or speak with someone who understands, we’re here to help. Our resources provide the information and support you need to make the best decisions for your health. You don’t have to face this alone—reach out today.
When your tricuspid regurgitation advances, it can be serious. Stay informed and take action.
Phone: 949-250-2012
Toll free: 888-713-1564
References
- American Heart Association. Heart Valves and Circulation. www.heart.org/en/health-topics/heart-valve-problems-and-disease/about-heart-valves/heart-valves-and-circulation. Accessed June 13, 2024.
- American Heart Association. Roles of Your Four Heart Valves. www.heart.org/en/health-topics/heart-valve-problems-and-disease/about-heart-valves/roles-of-your-four-heart-valves. Accessed June 13, 2024.
- Topilsky Y, et al. Clinical Outcome of Isolated Tricuspid Regurgitation. J Am Coll Cardiol Img. 2014;7:1185-1194.
- U.S. Census Bureau (2021). American Community Survey 1-year Estimates.
- Cahill TJ, et al. Community prevalence, mechanisms and outcome of mitral or tricuspid regurgitation. Heart. 2021;107:1003-1009.
- MedlinePlus; Tricuspid regurgitation. https://medlineplus.gov/ency/article/000169.htm. Accessed on 2.10.2025.
- Welle GA, et al. New Approaches to Assessment and Management of Tricuspid Regurgitation Before Intervention. JACC: Cardiovascular Interventions 2024;17: 837–58.
- CardioSmart American College of Cardiology. Treatment https://www.cardiosmart.org/topics/tricuspid-regurgitation/treatment Accessed on 2.10.2025
- Stocker TJ, et al. Burden of heart failure in patients with tricuspid regurgitation and effect of transcatheter repair on different subdimensions of quality of life. J Am Heart Assoc. 2024;13:e034112.
- Hahn RT. Tricuspid Regurgitation. N Engl J Med. 2023;388:1876-1891.
Important Risk Information
Edwards EVOQUE Tricuspid Valve Replacement System
Who can be treated:
The EVOQUE tricuspid valve replacement system (the EVOQUE system) is approved for treating patients with symptomatic severe tricuspid regurgitation (TR) for the improvement of health status. TR is a condition in which the tricuspid valve on the right side of the heart doesn't close properly. When the valve does not fully close, blood flows backward from the lower chamber (ventricle) into the upper chamber (atrium) making the patient's heart work harder to move blood through the valve. Patients should work with their doctor and a specialized Heart Team to determine if the patient is a suitable candidate for the EVOQUE valve.
Who should not use:
The EVOQUE system should not be used in patients who:
- Cannot take blood thinning medications
- Have an active infection in the heart or elsewhere
- Have an untreatable allergy to nickel or titanium
If used in the patients mentioned above, it will not work properly and could make you feel sick or even cause death.
Warnings:
How long your tissue valve will last depends on many patient factors and medical conditions. Follow all care instructions to ensure the best possible results. The Edwards EVOQUE valves have been tested in a laboratory to mimic 5 years of use without failure. Regular follow-ups will help your doctor know how your EVOQUE valve is working.
- Follow all care instructions to ensure the best possible results. Regular follow-up is advised to evaluate the performance of your device
- Blood thinning medication may be necessary after valve replacement with the EVOQUE system. Your doctor should prescribe this and other medical therapy per standard guidelines.
The safety and effectiveness of the transcatheter heart valve is not known for patients:
- Who are dependent on their pacemaker without other pacing options
- Who had a pacemaker implanted within the last 3 months before the valve implantation procedure
- Who have severe pulmonary hypertension not managed by medication
- Who have severe right ventricular dysfunction
Precautions:
Precautions Prior to Use
Seeing a specialized doctor on a Heart Team will ensure you are evaluated for all treatment options. They will consider factors about your health to decide the most appropriate treatment option for you.
Your doctor will consider these factors:
- Your medical history
- Your age
- Your current health status
- Your ability to undergo the procedure and recover from it
- The overall condition of your heart
General Precautions
- Problems with the electrical pathway of your heart that require a pacemaker may occur before, during, or following implantation of the EVOQUE valve
- Talk to your doctor about risk of infection and needing antibiotics if you require a dental procedure after your heart valve replacement
- Long-term durability has not been established for the EVOQUE valve. Clinical data is reflective of short-term follow-up, and regular medical follow-up is advised
Potential Risks
As with any medical procedure, there is a possibility of risks.
The most serious risks associated with the procedure are:
- Death
- Stroke
- Serious bleeding (with the potential to be given blood)
- Problems with the electrical pathway of your heart that requires a pacemaker
- Unplanned repeat procedure, hospitalization, or surgery
- Major vascular complications
- Permanent disability
Additional potential risks include:
- Abnormal lab values
- Abnormal low or high blood pressure
- Additional cardiac surgery, vascular surgery, or intervention, including removal of the transcatheter heart valve
- Allergic reaction
- Anemia
- Blood leak around the valve
- Chest pain
- Collection of fluid or blood around your heart
- Damage to blood cells
- Damage to the swallowing passage (esophagus), with possible puncture or narrowing
- Damage to the valve or deterioration (wear, tear, fracture, leaflet thickening, stenosis), malposition, clotting, movement or embolization of the valve, which might require removal of the valve
- Failure to retrieve any EVOQUE system components
- Fluid buildup in your lungs
- Having an abnormal particle (air or blood clots) floating in the bloodstream or attached to an object, including the valve
- Heart attack or heart failure/decreased heart pumping
- Incorrect position of valve or valve movement
- Infection in your heart, blood, or other areas
- Interference/damage with an existing permanent pacemaker or defibrillator
- Irregular heart rate
- Kidney failure
- Nausea and/or vomiting
- Nerve injury, paralysis or neurological symptoms, including problems with movement or walking
- Organ failure, including heart failure
- Pain, inflammation, or fever
- Right ventricular outflow tract (RVOT) obstruction
- Severe bleeding or fluid in or around the heart or in the body that could require a transfusion or surgery
- Skin burn, injury or tissue changes due to exposure to X-rays
- Sudden or unexpected loss of heart function
- Swelling
- Trouble or inability to breathe
- Valve regurgitation (new or worsening tricuspid, aortic, mitral, or pulmonary)
CAUTION: Federal (United States) law restricts this device to sale by or on the order of a physician.